Why the novel coronavirus is much worse than the flu
COVID-19, the novel coronavirus, is continuing to sweep through the world at pandemic levels, and many governments are implementing strict social-distancing guidelines to be followed to mitigate its spread. However, when a majority of the symptoms for this virus are comparable to the seasonal flu, it is understandable why many Americans and people around the world view COVID-19 as “just a bad flu” and view the drastic actions taken by governments as extreme and unnecessary. This, unfortunately, could not be farther from the truth as COVID-19 differs vastly from the seasonal flu from its biology to its severity. These differences have extreme implications on the way we as people should view and respond to this pandemic.

January 25, 2020: Red Cross Hospital in Wuhan, China
Biology
The initial cases of COVID-19 in Wuhan, Hubei Province, China in late 2019 appeared to only have been individuals with some connection to live animal markets. This was due to the fact that COVID-19, much like the others in its family of viruses like MERS and SARS, is a virus found in animals that develops a mutation to allow it to spread from the infected animal to people (the likely candidates for the origin of this virus are thought to be bats).2 Since only those in contact with infected animals were getting sick, officials believed that Coronavirus could only be acquired from animals and that person to person transfer was not yet possible. For example, rabies can only be contracted from being bitten by an infected animal (or other exposure to bodily fluids) while interacting with an infected person would not get you sick.
However, soon cases in China began popping up where the infected individual did not have a link to these live animal markets or have any other possibility of interacting with the infected animals. This led to the conclusion that the virus had mutated again to allow it to spread from person to person.2 These mutations occur randomly, and while the virus itself works to correct them, some get past the virus’s proof-reading, creating new, potentially more aggressive strains of the virus. Currently, scientists have identified two strains of COVID-19 that have been contributing to the epidemic: L type and S type (where L type is found in around 70% of cases and is believed to be more aggressive due to this, but researchers are still unsure).8
Mutations are common in most viral infections, including influenza (seasonal flu) strains, so why does this matter? Influenza has been studied and well researched for many years, and there are already effective treatments and vaccines that have been developed. Therefore, new influenza strains are much easier to understand, vaccinate, and treat than new COVID-19 strains where scientists are still scrambling to determine methods for treating and vaccinating the original strain of the virus. Similarly, the human body is also more familiar with influenza strains and has established immunities to some of these various strains. However, COVID-19 is completely unknown to our bodies until infection or vaccination (which will take around 17 months before it is proved to be effective and readily available based on hopeful estimates).6 As this virus spreads to more and more people, the likelihood of mutations becomes more common, and this opens the door to the potential creation of more severe strains of COVID-19. This is a major reason why slowing the spread of the disease can help scientists establish effective vaccines and treatment methods before the creation of new strains make them ineffective.
Severity
If you have been tracking the impact of this virus around the world, then you have also likely seen various sources reporting death rates and hospitalization rates that are different day to day. The aggressiveness of the virus is not likely changing this frequently, and instead factors like the awareness of COVID-19, access to testing supplies, and availability of medical supplies can influence the tracking and treatment of this virus. Estimates from the WHO (World Health Organization) place mortality rates in various regions around the world to be between 0.25% to 3.0%.5 Areas with a high density of cases are much more likely to have higher mortality rates (proportion of cases ending in death) due to the strain placed on health centers to treat their patients with limited supplies.5 However, current data suggest that the mortality rate of coronavirus is higher than that of the seasonal flu, which rather consistently kills around 0.1% out of those who show symptoms of the viral infection in the United States.1 Refer to the graphs below to see the comparison of the CDC’s hospitalization and death statistics in the United States between the 2019-2020 flu season and COVID-19’s impact as of March 16.7
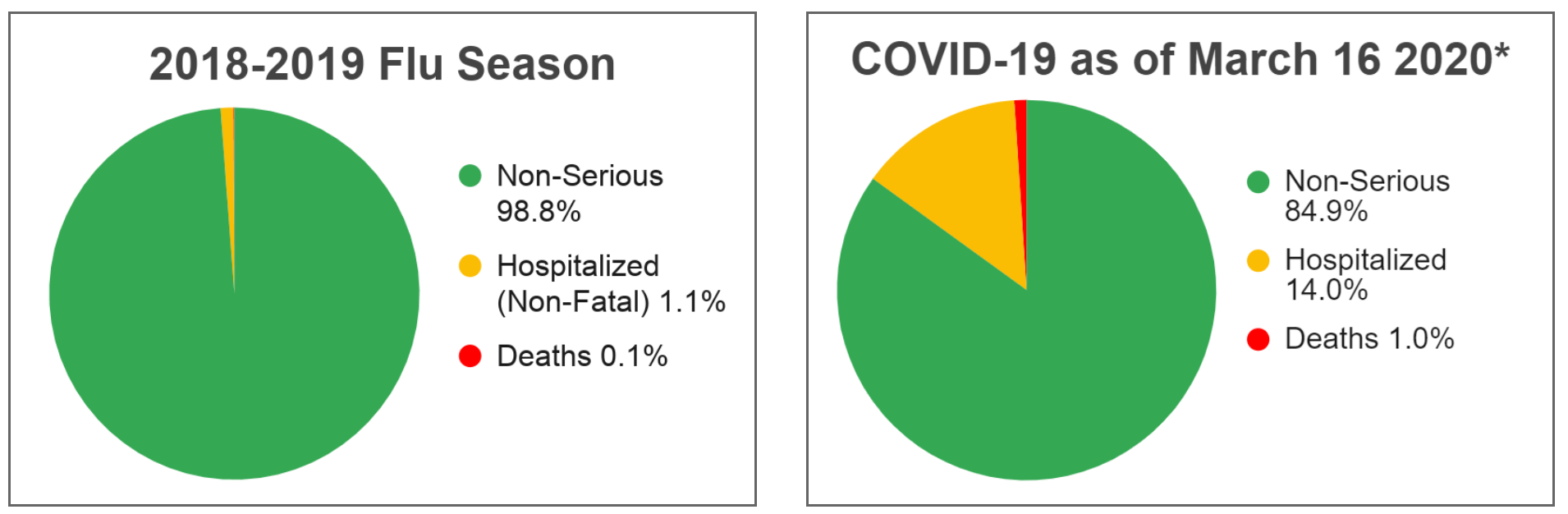
*COVID-19 statistics could be inaccurate due to underreporting
Another factor that might set COVID-19 apart from the seasonal flu is how it is spread. Both COVID-19 and the flu can be transmitted to a person through the contact of droplets (from an infected individual coughing, sneezing, or talking), but researchers believe that COVID-19 could also spread through the airborne route.3 A study conducted on this phenomenon found that COVID-19 could remain in the air for up to three hours.4 If that weren’t enough, the virus can survive up to 24 hours on materials like cardboard while surviving as long as 3 days on plastic and stainless steel surfaces.4 This makes it easier for the virus to spread from person to person, resulting in many more cases. These increased cases will lead to increased strain on hospitals and, as discussed above, significantly higher mortality rates.
The Good News
Hopefully, by now it is clear why COVID-19 differs from the seasonal flu in ways that make it a much more serious threat. While researchers and clinicians are still determining consistent methods for treatment and developing a vaccine, we still do have options to reduce the impact of this virus today. We have access to a “social vaccine” that can reduce our chances of acquiring the disease and spreading it to more people. How do we get this social vaccine? We stay at home and minimize our interactions with other people, especially when we feel sick. If all of us are able to follow these practices, the rate of spread of COVID-19 will decrease. Again, as the spread is reduced, so is the strain placed on hospitals and ultimately, the mortality rates will also be kept to a minimum (refer to the graphic below). The threat that COVID-19 poses is real and while our understanding of this new virus is limited, research can confidently say that this is much worse than the seasonal flu and deserves to be taken seriously.
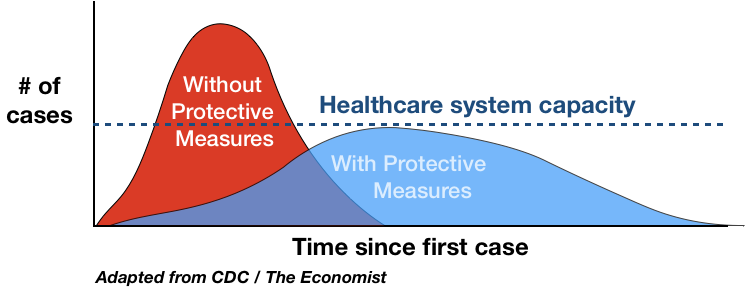
“Flattening the Curve”: Through limiting social interaction there is less strain put on the health system and lower mortality
References
- “2019-2020 U.S. Flu Season: Preliminary Burden Estimates.” Centers for Disease Control and Prevention, Centers for Disease Control and Prevention, 13 Mar. 2020.
- “Coronavirus (COVID-19).” National Institutes of Health, U.S. Department of Health and Human Services, 18 Mar. 2020.
- “Coronavirus Disease 2019 vs. the Flu.” Edited by Lisa Lockerd Maragakis, Coronavirus Disease 2019 vs. the Flu | Johns Hopkins Medicine, 18 Mar. 2020.
- “Coronavirus Resource Center.” Harvard Health, Harvard Medical School, 18 Mar. 2020.
- “Early Release - Case-Fatality Risk Estimates for COVID-19 Calculated by Using a Lag Time for Fatality - Volume 26, Number 6-June 2020 - Emerging Infectious Diseases Journal - CDC.” Centers for Disease Control and Prevention, Centers for Disease Control and Prevention, 18 Mar. 2020.
- Grenfell, Rob, and Trevor Drew. “Here's Why It's Taking So Long to Develop a Vaccine For The New Coronavirus.” ScienceAlert, 17 Feb. 2020.
- “Severe Outcomes Among Patients with Coronavirus Disease 2019 (COVID-19) - United States, February 12–March 16, 2020.” Centers for Disease Control and Prevention, Centers for Disease Control and Prevention, 18 Mar. 2020.
- Tang, X, et al. “On the Origin and Continuing Evolution of SARS-CoV-2.” OUP Academic, Oxford University Press, 3 Mar. 2020.